The mouth is the gateway to the entire body. It’s a connection between dentistry and medicine. Routine dental visits are crucial not only for oral health, but also screening for general health concerns because the majority of people visit their dentist at least twice per year which is typically more often than their general physicians. One of the most important things we evaluate is the airway. The airway provides a path for air in and out of the lungs, where it supplies oxygen to the brain and body. We’re meant to breathe through our nose so that it can filter out the dirty air. If not, then inflammation of the airway, respiratory infections, enlarged tonsils or obstructed airway can result. An open airway is important for sleep, rest for the brain, and overall growth and development. For pediatric dentists, a healthy and open airway is crucial for dental treatment with sedation because many of the medications given can cause a temporary depression in the respiratory drive for the patient, with potential severe outcomes in a compromised patient.
Sleep apnea (or sleep disordered breathing) is a dysfunction of breathing during sleep. It can be an actual airway obstruction or failure of the brain to send the right signals telling the body to breath. Sleep apnea is characterized by abnormal patterns of breathing such as repetitive starting and stopping, snoring, abnormally slow or shallowed breathing, or breathing through the mouth rather than the nose. A person can actually stop breathing for at least 10 seconds before “waking up” to catch a breath. The brain and entire body require sufficient oxygen to function. When that is constantly disrupted, it can have detrimental long-term effects such as high blood pressure, stroke, heart disease, diabetes, behavior problems (like ADHD), etc. Other signs that a child is having some sort of sleep apnea includes restless sleep, waking up multiple times during the night, wetting the bed, morning headaches, constant nasal congestion, chronic bad breath, trouble focusing in school or falling asleep in class, etc.
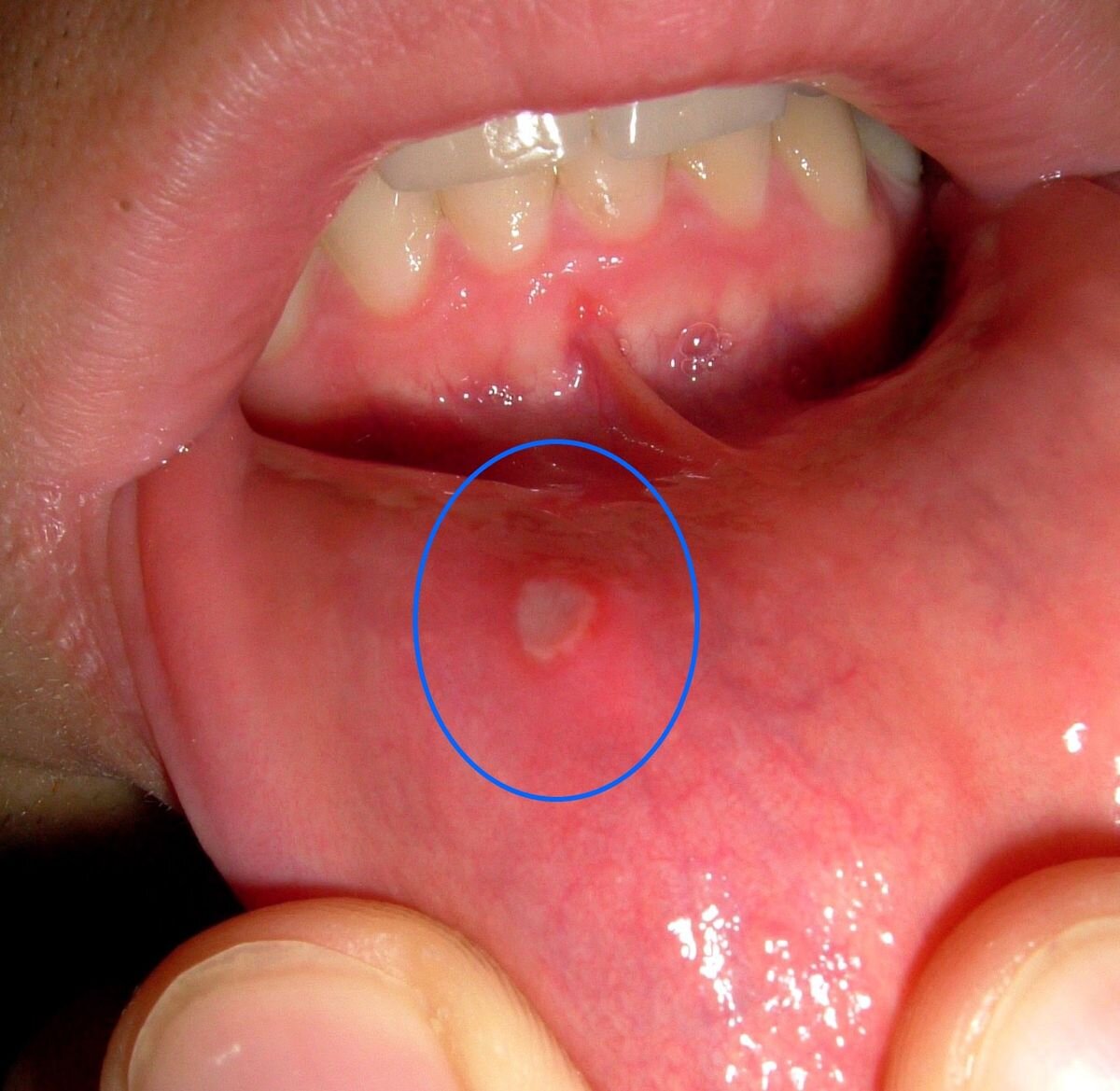
Our doctors at Smiles for Kids screen all of our patients for airway concerns at every dental visit. We evaluate the TMJ, head and neck muscles, mouth opening, tongue, teeth, throat, tonsils, and overall oral health. There are many clues in the mouth that can signal potential problems with the airway and sleep disordered breathing such as clenching/grinding, pain in the TMJ, large tonsils or adenoids, bite issues (or “malocclusions”), narrow palate, open mouth posture, cavities, gum disease, dry mouth, etc. Any of these signs will lead us to ask questions about the patient’s quality of sleep and a history of signs or symptoms previously mentioned.
There is much to consider before treatment of sleep apnea, and we work closely with our medical community, Ear Nose and Throat doctors (ENT) and Myofunctional Therapists for proper referral and evaluation. Dental treatment may include night guards or appliances such as a palatal expander. Expanding the palate can create more room for the teeth and the tongue, open the nasal passages, allowing for more air exchange and more relaxed muscle posture during sleep. Are you or your child experiencing any of the signs or symptoms of sleep apnea? Ask us more about it at your next dental visit!